Prescribing Debates in Home Dialysis

On a fairly regular basis, we see debates about prescriptions, or how dialysis prescriptions are “supposed” to look on our (and other) social media. There is controversy at every level in the industry about the “right” way to do things. There are also absolutely multiple “camps” of beliefs among providers, nurses, and patients—and tons of variations in practice.
I commented on one of our message board posts about prescription differences recently, and it was suggested that I turn my comment into a post of its own. Sure. No problem… This is where I am going to go ahead and remind everyone that medicine is both an art and a science.
Let’s Start with PD?
A lot of people firmly believe in a PD-first approach, but many will begin to disagree over whether training (and ultimately prescription) should be for manual and then automated—one or both?
Dose is another topic. One group inevitably argues that incremental PD is the “right” way, with an emphasis on utilizing and preserving residual function for as long as possible. Others favor full-dose PD at onset, with the option to “maybe back down” at a later time. Add in the mumbled voices from the back that inform everyone that PD isn’t very good at removing B2M and that can only be a trade-off with the benefits of residual function preservation for so long.
Things Are Even More Chaotic on the HD Side
A lot of folks lately seem really into the idea of treating home dialysis like it’s standard in-center treatment, just…at home. Some patients have equipment and sufficient supplies at home to run safer treatments and completely avoid 2-day gaps—but are encouraged to run on a thrice weekly schedule, with no additional time. I find this concerning.

If a home HD treatment is performed in the exact same way as an in-center treatment…is there any health benefit other than a cozier location? Does that fall into the realm of personal choice? Are the chances of an emergency happening (you know, the scary things like sudden cardiac death) just as high if not higher when this is being done? I’m not sure. It really worries me for our industry though.
Patient blood flow rates at home are always a hot topic. I was
speaking with another nurse recently and we discussed the highest
prescribed BFR we’d ever seen. Mine was 550 on 14g needles. Hers
was 600! Both of these numbers are completely shocking and  outrageous
to me. Just thinking about them gives me anxiety!
outrageous
to me. Just thinking about them gives me anxiety!
One reason I left clinical nursing was the ethical dilemma I had over frequent orders calling for high BFRs after reading John Agar’s blog, Don’t Flog the Fistula. I don’t think numbers like that belong at home—or in-center. I see the concepts described in that original blog and have been deeply affected by them.
Some clinics encourage rigid home HD treatment schedules—even to the point where total ultrafiltration volume is pre-set to an average, and patients do not understand how to make adjustments, regardless of their fluid status. Hypotension from pulling too much fluid should never happen at home—or in-center—and these scenarios seem like a perfect storm for exactly that.
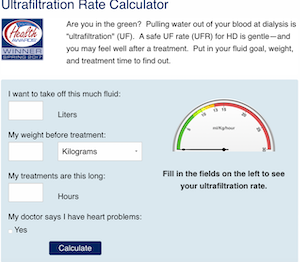
There are also patients who do not know (or are not permitted) to lengthen their treatment time for the purposes of lowering their ultrafiltration rate (UFR). These are fundamental concepts. Being aware of UFR and the dangers of organ stunning is something we have made quite easy for patients to do from home—and it’s FREE. Patients deserve this information.
In some programs, patients are actively encouraged to do more frequent treatments and have different schedules based on what works best for them. We talk to patients who treat every other day, and we talk to patients who treat every day. Everything in between exists, too.
There are people who have busy lives and have managed to work out how to have multiple dialysis order options—depending on what they feel like and have time for. There can be long home HD treatments, short home HD treatments, and “just right” home HD treatments. Often these same patients have been shown how to adjust for time and UFR and understand the reasons for doing so.
Some home HD programs do not allow patients to treat without partners, or do nocturnal HD even with a partner—and encourage so-called “caregivers” (we prefer “care partners”) to be very actively involved in treatment—more so than the patient, even when the patient is capable. This can harm couple relationships, as co-dependence and burn-out creeps in. At least that’s what I’ve seen. Established home programs with well-trained nurses speak fondly of nocturnal home HD as a “gold standard” in the good old days and reminisce constantly about how the treatment was so good, “we had to give them back phosphorus!”
“More is always better” is just as incorrect as "less is always more." Neither statement takes into account the human involved. People are not sets of labs. Who are each of your patients? What do they value? What do they want? What are they willing to do? How do they feel about what is happening? How can we help meet those needs?

A “correct” dialysis prescription is specific to individual preferences, physiology, needs, and wants. Different patients have different goals of care and primary concerns and deserve to weigh these kinds of decisions in the most informed manner possible. We have the flexibility in home dialysis to customize and be creative for the sake of quality of life. This is the art part. The freedom to do these things in an individualized way: to analyze, tweak, debate, and perfect for each person is one of the under-lying goals of home therapies.
If a person’s focus is only on quality of life and “enjoying life” is defined by not doing a lot of treatment, then sure, one option is to reduce treatment time and/or frequency and let symptoms be the guide. A person can replace just enough function to feel well enough to carry about with their business as they had been. There is nothing wrong with that, as long as the patient is the one weighing the pros and cons with a clear and informed mind. This might be a fantastic choice for some patients—and a disastrous one for others.
A different person might want to focus on systemic preservation and physiologic stability. That person might really value living for as long as possible with fewer irreversible complications. They might want to not limit their diet at all, ever. If that’s the case, then slower/longer/more frequent treatments make the most sense.
Flexibility in practice is the only real way to meet the
needs of all of the patients in a home population. Part of the
art is finding a treatment “sweet spot” that allows patients to live
life to the fullest on their own terms. When at home, we should err on
the side of limiting complications always. This means really
incorporating things like low UFRs, longer treatment, slower BFRs, more
frequent treatment, etc., into our culture.
This means really
incorporating things like low UFRs, longer treatment, slower BFRs, more
frequent treatment, etc., into our culture.
Anyone want to pick a hill to advocate on yet? If so, please do so in comments. ☺


Comments
Diane
Apr 16, 2024 10:30 AM
Tina M Renfroe
Apr 05, 2024 3:52 PM
Nancy Verdin
Apr 04, 2024 8:54 PM