Hope for Health Equity in Home Dialysis

The Past
When dialysis machines were in short supply and “life or death committees” had to choose which patients would be allowed to get this new treatment based on their value to society, there was inequity in who was offered this new treatment. Most of those chosen were young, healthy males, who were well educated, employed and insured or who had funds to pay for the costly treatment before it was government-funded. At that time, most people did hemodialysis (HD) in hospitals, but a large percentage—about 40%--did HD in their homes.
Once Medicare began to cover dialysis in 1973, patients of all ages, including those with serious illnesses were admitted to hospital-based outpatient dialysis clinics. Shortly thereafter physicians moved dialysis clinics out of hospitals and clinics started being acquired by companies that provided mostly in-center HD. Although there was some PD in the 1960s, it wasn’t widely available. As more clinics outside hospitals opened, the number of patients on home dialysis declined dramatically until fewer than 10% of patients were doing any type of home dialysis.
Then in 2019, the Advancing American Kidney Heath Executive Order set lofty goals: (1) to reduce the number of patients developing kidney failure 25% by 2030 and (2) for 80% of patients to have a kidney transplant or to be on home dialysis by 2025. The CMS Center for Innovation (CMMI) developed a plan to reach these goals. To promote home dialysis, it assigned a percentage of clinics to be in the ESRD Treatment Choices Model whether they had a home program or not. Those clinics that improved the percentage of home patients would get points toward higher reimbursement. To address inequity in home dialysis, CMS has now changed the ETC Model to award more points to clinics that achieve targets and have more home patients who are dual eligible (Medicare/Medicaid) or who get the Part D low income subsidy. Read the ETC Model’s history and learn about new ESRD QIP measures that may help to address health equity in home dialysis here.
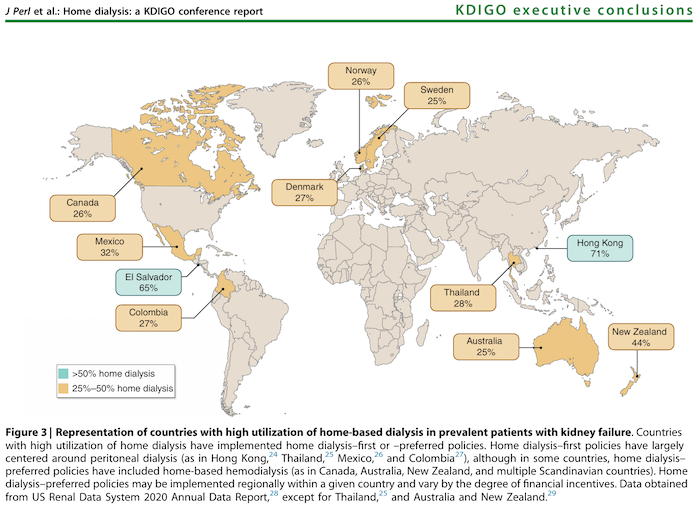
A 2023 report of conclusions from the Kidney Disease: Improving Global Outcomes Home Dialysis Controversies Conference has a map showing home dialysis percentages in 11 countries outside the U.S. Data for this map are from the USRDS 2020 Annual Data Report (2018 data):
Countries with a PD-centered “home dialysis first” approach include Hong Kong-71%, Thailand-28%, Mexico-32%, and Colombia-27%
Countries with a “home dialysis preferred” with PD and home HD include Canada-26%, Australia-25%, New Zealand-44%, Denmark-27%, Norway-26%, and Sweden-25%.
The report also discusses four economic drivers of home dialysis use:
Funder (Payer) – Does funding (government/other) or policies improve availability of home dialysis?
Dialysis provider – What model of care do they use, profit or not-for-profit?
Nephrologist – Are they fee for service or salaried, do home dialysis incentives or disincentives affect their pay, and do they have any ownerships in the dialysis clinic?
Patient – Can s/he pay out-of-pocket costs, be off work for training and appointments, and keep his/her job and income in spite of burden of treatment?
In comparison to those other 11 countries with at least 25% of their patients on home dialysis, the only half that percentage—only 12.5% of U.S. patients were on home dialysis according to the USRDS 2020 Annual Data Report.
The Present -- Data Related to Home Dialysis
Chapter 2 in the United States Renal Data System’s 2023 Annual Data Report on home dialysis reports patient characteristics for incident home dialysis patents and patients on home dialysis one year after ESRD.
Race: Asian and White patients were more likely to be initiated on home dialysis and to be on home dialysis at one year after ESRD than Black, Hispanic or other patients.
Age: Younger patients under age 65 were more likely than those 65 and older to start dialysis with home dialysis and to be on home dialysis at one year after ESRD.
Insurance: Those with an employer group health plan as their primary payer were more likely to be on home dialysis than those with Medicare/Medicaid.
Location: At initiation, rural patients were only slightly more likely to be doing home dialysis, but a year after ESRD, there was a wider difference with rural patients more likely to be on home dialysis than urban ones.
Area Deprivation Index (ADI): Dialysis patients living in areas with lower income, education, employment, and poorer housing were less likely to be doing home dialysis.
On this latter point, the Health Resources and Services Administration developed that index more than 30 years ago. You can use the Neighborhood Atlas® mapping program to see color coded ADI rankings on a map of the U.S. or any state down to the census block. The maps are based on 2014-2018 American Community Survey responses.
The 2021 National Healthcare Quality and Disparities Report (NHQDR) described racial and ethnic disparities, disparities in access to care and quality of care for different populations and discussed disparities related to diabetes and kidney disease. In 2022, CMS called on leaders in the healthcare industry to commit to advancing health equity and work with CMS to identify and share best practices to address inequities. A fact sheet lists 6 pillars to “promote quality outcomes, safety, equity, and accessibility for all individuals, especially for people in historically underserved and under-resourced communities:
Advance equity
Expand access
Engage partners
Drive innovation
Protect Programs
Foster excellence”
The Challenge
USRDS national data reflects inequities in what categories of patients are more likely to use of home dialysis. There may be multiple reasons. Some things I’ve heard that may adversely affect home dialysis utilization include::
From nephrologists
Lack trust in patients to do dialysis as prescribed unsupervised at home;
Skewed perceptions of who will and will not do well on home dialysis that could be related to unconscious bias;
Perception that home patients take more of their time than seeing all in-center patients rounds during a dialysis shift or two.
From dialysis companies
Perception that home HD is more costly than PD or in-center HD;
Limit home dialysis programs—according to USRDS in 2021:
45.1% of clinics had no certified home dialysis program
11.4% of clinics had a certified dialysis program but no home patients
42.9% of clinics had a certified home program treating patients
From patients
Lack of knowledge prior to dialysis (and even after starting in-center dialysis) about other options besides the default—in-center dialysis
Lack confidence in their ability to self-manage
Fear needles and placing them (HD) or have body image concerns (PD)
Fear making a mistake and having a medically unsupervised emergency.
The Future
We will see what the future holds in store for home dialysis. The ESRD Quality Incentive Program is a system of payment based on performance on certain measures and improvement on those measures. In Payment Year (PY) 2026 based on data collected on measures during calendar year (CY) 2024, dialysis clinics will get up to 10 points on a new measure called Facility Commitment to Health Equity. How many of those 10 points a clinic will get is based on an attestation of their organizational competency in 5 domains of health equity. To learn more, read about this fact sheet.
The Final Rule for ESRD PPS, AKI, QIP, and the ETC Model published on November 6, 2023, included two new health equity QIP measures. Clinics will collect data in CY 2025 for PY 2027:
“Screening for Social Drivers of Health, a reporting measure
Percentage of patients at a dialysis facility who are 18 years or older screened for all five health-related social needs (HRSNs) (food insecurity, housing instability, transportation needs, utility difficulties, and interpersonal safety).
Screen Positive Rate for Social Drivers of Health, a reporting measure
Percentage of patients at a dialysis facility who are 18 years or older screened for all five HRSNs, and who screen positive for one or more of the following five HRSNs: Food insecurity, housing instability, transportation problems, utility difficulties, or interpersonal safety.”
One big question is whether a greater focus on health equity will spur dialysis clinics to help patients choose a treatment that fits for them. MEI created the My Kidney Life Plan decision aid. Nephrologists or staff in their office can share this with CKD patients who are nearing the need for dialysis. This tool helps a patient choose what they value and see which of the options for dialysis fit with those values that are important to THEM. MEI has a wealth of information and resources on Home Dialysis Central and the Home Dialysis Central Facebook group that MEI administers and monitors answers questions and provides support to patients on home dialysis or considering it. We have a way to go to reach the target set by the Advancing American Kidney Health executive action. As the Chinese proverb says, “A journey of a thousand miles begins with a single step." Let’s take that step by working to overcome our biases to give all who have kidney failure a chance to have a fuller and more productive future.


Comments