What is an Ejection Fraction, and What Does it Mean to You?
Article by Prof. John Agar, Geelong, Australia
(Revised for Home Dialysis Central—March 2009)
A U.S. patient recently asked me about hearts, dialysis, and left ventricular function. My answer mentioned the ejection fraction and he asked me "What's that?"
Well, I think it is a useful test, and it allows me to discuss (yet again) my pet topic: dialysis time and frequency.
What's an ejection fraction?

The left ventricular (LV) ejection fraction (EF) is a nice 'number' for a dialysis doctor like me to know. Why? Because the LVEF tells me a lot about how good (or how poor) the function of the heart is.
When I think about volume in a dialysis patient—especially when the BP is low—I want to know:
- Is the BP low because the dry weight has been set too low? This is common when you gain true body weight, and we are trying to keep to a "lower-than-it-should-be" dry weight by sucking too much fluid out on dialysis. Or...
- Is the dry weight not the cause of the low BP, but rather, the BP is low because the heart is struggling to pump sufficiently "oomphily"? (A heart that cannot pump efficiently cannot drive, or sustain, an adequate BP.)
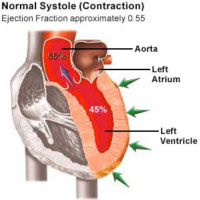 When I try to interpret volume and make good decisions, it is always nice to know how strong the heart is. Knowing the
LVEF
can be a great help. A normal
LVEF
is when 55-70% of blood volume in the left ventricle—the main pumping chamber of the heart—is
ejected
(pumped) with each heartbeat.
When I try to interpret volume and make good decisions, it is always nice to know how strong the heart is. Knowing the
LVEF
can be a great help. A normal
LVEF
is when 55-70% of blood volume in the left ventricle—the main pumping chamber of the heart—is
ejected
(pumped) with each heartbeat.
The heart doesn't pump all its contained blood when it contracts; only a bit over half is "ejected" with each beat. But a poor LV may eject well less than 20% ...and that's not a very efficient heart.
What an LVEF means
If the EF is good, then I also know that:
- Your heart is strong and can stand some extra filling
- Adjusting the dry weight "up" is safe for your heart...and almost certainly the right thing to do.
If the EF isn't good, and there are grades of "not good" set by the New York Heart Association (from Grade I to Grade IV with IV being the worst), it complicates the approach to fluid management.
Loading up your circulation with extra fluid may just further over-stretch the already-stretched LV. This risks pushing the LV over the edge of Starling's Curve.

Starling's Curve is a key cardiac concept! If the LV is over-stretched—and Starling's Curve exceeded—your heart will simply throw up its hands in despair, say "stuff this ... I've had enough," and pump even less efficiently.
Think of a rubber band or a balloon. Stretch it a little and it will spring back to its original size. But overstretch it, and it won't fully recoil. Over-fill an already tired and stretched LV, and it will get worse.
So...over fluid-filling a poorly-working LV may make an already over-stretched (dilated) LV fare even worse. This may cause the BP to drop even more rather than rise in response to the fluid load.
Raising the dry weight or letting you drink more fluid is quite counter-productive if there is a poor EF; hence my interest in knowing the EF when I seek to choose the right course of action.
What can be done for a poor EF

While some drugs can help the LV to pump better, avoiding over-stretch is utterly important. This is the most cogent reason for more frequent (daily) dialysis.
In daily dialysis, there are two key advantages:
- Less time between dialysis treatments for fluid gain
- Less fluid weight gain: 1 day of fluid gain vs. 2 or even 3 days gain with standard hemodialysis (HD)
Less time between treatments + less fluid gained = less LV overstretch.
Less LV overstretch = less stress on the rest of the heart.
Less stress on the heart = less cardiac risk and a lower risk of death.
This reduced 'stress' on the LV translates into a huge advantage. The chance of a poor EF is higher if the heart is a 'dicky heart' to begin with...as is the case with many patients with a long lead time into CKD, and where there has been high blood pressure.
Fluid removal rate counts
But...there's more. Slowing the rate of fluid removal is important, too. Some... and there are no prizes for guessing who they might be...believe that the fluid removal rate is just as important—and often more so—than the frequency (daily dialysis). Why?
Rapid removal of fluid drops the BP. Those who have had "dialysis flats" know this all too well. A fall in BP for an already struggling and failing LV is like shocking the already shocked! It is a "double-whammy".
As the BP falls, the perfusion (blood flow) to the coronary arteries that supply the heart muscle with blood also falls sharply. So, the oxygen supply to the heart muscle falls. This rapidly worsens the situation for the LV.
The role of thirst

The rapid removal of fluid that drops the BP during dialysis does so by dropping the blood volume sharply. And a fall in blood volume turns on thirst!
Thirst is a hugely powerful, primitive drive ...and primitive drives (they are, after all, survival mechanisms) are so strong that they are almost impossible to resist! Turning on the thirst drive (by a rapid fall in blood volume) irresistibly drives you to drink as soon as possible after dialysis. It is the body's way of trying to restore the blood volume.
So, a standard HD patient is in a no-win state. The thirst drive overcomes the fear of staff threats and in goes the fluid! An un-thinking dialysis staff may berate you for drinking too much between sessions but, commonly, this is not something you can help.
No...it's not your fault—it's ours!
Infrequent, sudden—or both—fluid removal done in short, standard HD will trigger your (irresistible) thirst drive. Once you are thirsty on standard HD, you are set up to fail. You'll gain too much weight before your next treatment. It is a vicious cycle.
Answer – slow the rate of fluid removal!
Answer – lengthen the dialysis session! Then the rate and amount of blood volume contraction can be reduced.
Longer dialysis at the centre is unpopular with patients—though it is our experience that, if clearly explained, patients are the least of the problem. In Australia, the mean dialysis time is now >4.5 hrs (270 mins), while in the U.S., it is only 211 minutes!
The greater problem is that it can be difficult to schedule and fund, even if the patient can be persuaded of the sense to it. But...
- This is a problem the 'system' has to solve.
- Scolding a patient never, ever works!
"Compliance" is not the issue
All scolding does is to put the patient off side and create "angst" between patients and staff. That is no solution. At the same time, the staff may decide the patient is hopeless, useless or "non-compliant" and shrug him or her off as a lost cause. This staff approach may be part of the reason why "compliance" is such an issue in the US and is so not an issue in Australia!
Why are U.S. patients said to be so "non-compliant" compared to their Australian "cousins"? In my view, it is because U.S. short, infrequent, thirst-driving, symptom-heavy dialysis regimes set them up to fail.
Slower, longer, gentler, more frequent dialysis—and following the treatment plan—are the best things anyone can do to protect the heart.
End of story!
I am a zealot for long, slow dialysis...but my zeal arises from trying to better understand dialysis physiology and from wanting the best for my patients' hearts!
Back to the beginning then: it is important to have a sense of what the EF is.
The EF is easy to measure by an echocardiogram. An echocardiogram is quick, cheap, painless and reliable. We do them once a year in all of our patients, as we know hearts can (and do) change.
The EF is a measure that should be 'computed' into our decisions about the right blood volume for any given patient, and the right responses to it.
References:
- Left Ventricular Ejection Fraction (LVEF) . Accessed March 2009.

