PD as a First Option
When your kidneys fail, dialysis can help you live, feel well, and have a good quality of life. You may have one or more transplants. You may try more than one type of dialysis. You can switch treatments if one you choose does not fit your life. So, which one should you try first?
With peritoneal dialysis (PD), you may be able to:
- Keep your remaining kidney function longer
- Have a better chance of getting a transplant
- Keep your job
- Start Medicare on day 1
- Care for kids or grandkids
- Learn the treatment quickly—and regain control of your life
- Get a fistula so you're ready for hemodialysis if you ever need it
The type of treatment you do will have a huge impact on your lifestyle—so the choice needs to be yours. Learn why PD may be a good first choice—if it will suit your needs, health, and lifestyle.
How PD Works
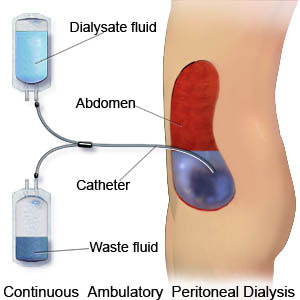
For PD, the sac that lines the inside of your belly (peritoneum) is used as a filter to clean your blood. A surgeon will place a soft, plastic tube (PD catheter) in your belly (or chest – link to Presternal article). Once it heals, a nurse will teach you to use the tube to fill your belly with sterile fluid (dialysate). In a few hours, wastes and excess water flow into the fluid. You drain out the used fluid and put in fresh a few times each day. This is an exchange.
You can do PD exchanges by hand—at meal times and bedtime. Each one takes about half an hour. Or, most people who do PD use a cycler machine at night to do their exchanges while they sleep. Since your blood never leaves your body, PD does not need needles.
Most people can do PD, but it may help you to know that:

- You may not be able to do PD if you had major belly surgery (a hernia repair, kidney transplant, or C-section should not stop you).
- You would need a clean, dry place to store 40 or so boxes of fluid bags.
- You would go to your clinic once a month for a check-up and blood tests.
- You'll need to keep pets out of the room and control the air flow when you do an exchange.
- The PD training nurse will teach you to care for your catheter each day and do each exchange step with care so you don't get an infection.
Keep Kidney Function Longer with PD
In most cases, kidneys don't lose 100% of their function when they fail—at least not right away. Having some kidney function can help you to:
- Feel better 1
- Have fewer diet and fluid limits 1
- Live longer 2,3

PD may help you keep some kidney function longer than standard hemodialysis (HD). 4,5,6 It is vital to do PD just as you are taught and avoid peritonitis infection, though. Peritonitis can cause a faster loss of kidney function. 7 Kidney function does tend to drop over time. If you choose PD, your kidney function will be checked with a 24 hour urine test until you stop making urine. You will need more PD as your kidney function drops.
PD May Boost Your Chance of Transplant
If you want a kidney transplant, PD may help. A study was done of more than 252,000 adult U.S. dialysis and transplant patients. The researchers found that people who did PD were about 50% more likely to get a transplant than those on standard HD. This was true even though the same number of people in both groups were listed for transplant. 9
PD is a good 'bridge' to transplant, since you do the treatments. With a transplant, you will need to take many drugs right way. Doing PD shows the transplant team that you can take care of yourself and will care for a transplant well.
PD is Work-friendly

How old are you? Each year, half of all new dialysis patients are under 65, or "working-age." Yet, fewer than 1 in 4 may keep a job after they start treatment. 10 For many, this means taking Social Security Disability, which pays only about 35% of what they earned before.
Job loss can push a household into poverty. But standard in-center HD, which is done by 91% of U.S. patients, is not work-friendly. Standard HD treatments are done during the work day. You may miss work because you feel "washed out" for hours after a treatment or have other symptoms.
PD is work-friendly. You can use a cycler at night, so your work days are free, or do an exchange in a clean room at work. Some PD patients do not even tell their employers that they are on dialysis. It is easy to travel on PD. And, PD is very gentle and going on most or all of the time. So, you won't have ups-and-downs in how you feel from day to day—and you may miss less work. Among more than 163,000 working-age people with kidney failure, those who kept their jobs were significantly more likely to have chosen PD or transplant than standard HD. 10
Keeping a job may also mean keeping an employer group health plan (EGHP). An EGHP will pay first for your first 33 months of PD. This means you should have fewer out-of-pocket costs to pay for (and more income to do it with).
Medicare Starts Sooner with PD
Paying for a chronic disease is stressful. It's good that Medicare pays for kidney failure treatment. But, if you do standard HD, Medicare starts with your 4th month of treatment. You have to pay for the first 3 months—and they can cost thousands, or tens of thousands of dollars. PD can help! If you start to train for PD before your 4th month, Medicare will pay from day 1. It can even be back dated to pay for your catheter, if you don't have a health plan. (Medicare pays 80%, so you will still want to have a second health plan to pay the rest.)
PD Makes Parenting Easier

Children can and do get used to a parent doing dialysis—it is just a part of life. But, if you have young or school aged kids, there will be days when a standard HD schedule will not fit your lifestyle. A child can be ill and need to stay home. There may be a play, concert, or sports game you would have to miss. It can be hard—and costly—to find childcare for school breaks and summer vacation.
The beauty of PD is that it can fit your needs. You can shift your exchange times a bit if you need to. So, you can go to those special events with your child. If you use a cycler at night, an extra-long tubing set will let you reach your child if he or she has a bad dream or a tummy ache.
PD is Easy to Learn
PD is easy to learn and to do. In most cases, you can learn it in a week or two. A PD nurse is on call 24 hours a day to answer your questions. You don't need a partner for PD, unless you can't lift the bags of fluid. If your hands or eyes don't work well, you may also need a helper. There are assist devices, though, and people who are blind can and do perform PD alone.
Learning to do PD puts you in charge of your life. It gives you back some of the control you lost when you found out you had kidney failure. And, feeling in control improves quality of life for people on dialysis. 10,11,12 A study of more than 4,000 patients found that a sense of control also boosted the chance of living longer and of getting a transplant. 13
Fistula First
Even if you choose PD, a day may come when you must switch to HD. For HD, you will need a vascular access—a way to get the blood to the filter (dialyzer). The "gold standard" type of access is a fistula. A surgeon links an artery to a vein in your arm. Fistulas are made only of your own tissue. They are the least prone to blood clots or infections, and can work well for decades.
Choosing PD first can buy you time to get a fistula, just in case. This means you may not need a central venous catheter (CVC). A CVC is a tube placed into a central vein in your neck or chest. It's best to not to have one; they have a high risk of sepsis (blood poisoning). In fact, a study of 5,500 people on dialysis found that those with CVCs were 54%-70% more likely to die than those with fistulas. 14
Medicare believes fistulas are vital to health and quality of life on dialysis. In fact, they started a "Breakthrough Initiative" called Fistula First. The whole kidney community now works to be sure that more fistulas are made.
Conclusion
You need to choose a treatment that will fit into your life, and let you feel your best. If it will work for you, PD can be a good choice as a first treatment for kidney failure.
References:
- The 'Bathtub' Presternal PD Catheter.
- Chandna SM, Farrington K. Residual renal function: Considerations on its importance and preservation in dialysis patients. Sem Dial May-June;17(3):196-201, 2004.
- Maiorca R, Brunori G, Zubani R, Cancarini GC, Manili L, Camerini C, Movilli E, Pola A, d'Avolio G, Gelatti U. Predictive value of dialysis adequacy and nutritional indices for mortality and morbidity in CAPD and HD patients. A longitudinal study. Nephrol Dial Transplant. Dec;10(12):2295-305, 1995.
- Termorshuizen F, Korevaar JC, Dekker FW, van Manen JG, Boeschoten EW, Krediet RT. The relative importance of residual renal function compared with peritoneal clearance for patient survival and quality of life: An analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD)-2. Am J Kidney Dis;June 41(6):1293-1302, 2003.
- Horinek A, Misra M. Does residual renal function decline more rapidly in hemodialysis than in peritoneal dialysis? How good is the evidence? Adv Perit Dial; 20:137-40, 2004.
- Misra M, Vonesh E, Churchill N, Moore HL, Van Stone JC, Nolph KD. Preservation of glomerular filtration rate on dialysis when adjusted for patient dropout. Kidney Int; Feb;57(2):691-6, 2000.
- Misra M, Vonesh E, Van Stone JC, Moore HL, Prowant B, Nolph KD. Effect of cause and time of dropout on the residual GFR: A comparative analysis of the decline of GFR on dialysis. Kidney Int; Feb;59(2):754-63, 2001.
- Shin SK, Noh H, Kang SW, Seo BJ, Lee IH, Song HY, Choi KH, Ha SK, Lee HY, Han DS. Risk factors influencing the decline of residual renal function in continuous ambulatory peritoneal dialysis patients. Perit Dial Int;Mar-Apr;19(2):138-42, 1999.
- Snyder JJ, Kasiske BL, Gilbertson DT, Collins AJ. A comparison of transplant outcomes in peritoneal and hemodialysis patients. Kidney Int;Oct;62(4):1423-30, 2002.
- Witten B, Schatell DR, Becker BN. Relationship of ESRD working-age patient employment to treatment modality. Poster presented at the American Society of Nephrology meeting, St. Louis, MO, October 31, 2004. (Abstract) J Am Soc Nephrol. 2004; 15:633A.
- Tsay SL, Hung LO. Empowerment of patients with end-stage renal disease--a randomized controlled trial. Int J Nurs Stud; Jan;41(1):59-65, 2004.
- Tovbin D, Gidron Y, Jean T, Granovsky R, Schneider A. Relative importance and interrelations between psychosocial factors and individualized quality of life of hemodialysis patients. Qual Life Res; Sept;12(6):709-17, 2003.
- Tsay SL, Healstead M. Self-care self-efficacy, depression, and quality of life among patients receiving dialysis in Taiwan. Int J Nurs Stud;Mar;39(3):245-51, 2002.
- Stack AG, Martin DR. Association of patient autonomy with increased transplantation and survival among new dialysis patients in the United States. Am J Kidney Dis;Apr; 45(4):730-42, 2005.
- Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int;Oct;60(4):1443-51, 2001.

