First, Do No Harm: As We Expand Home Dialysis, Put Patient Values First!

As most of us in the kidney community have heard, last week’s Executive Order to create the Advancing American Kidney Health Initiative (AAKHI) was big news for advocates who work to:

Slow chronic kidney disease (CKD) progression
- Increase use of home dialysis—peritoneal dialysis (PD) and home hemodialysis (HD)
Improve access to transplant
As always, the devil is in the details—and we don’t yet know what those details will be. Over the years, I’ve heard concerns that people will be railroaded into particular options, based on reimbursement. Thus far, this only seems to have happened with standard in-center HD! But, the potential for harm is present. Fellow advocates, please consider this post a rallying cry to ensure that people with kidney disease benefit from and are not harmed by whatever dialysis changes occur due to the AAKHI.
AAKHI Comment Period Until 9/16
Now that the AAKHI has been published in the Federal Register, there is a window for comment on the Medicare Program: Specialty Care Models to Improve Quality of Care and Reduce Expenditures until 11:59 p.m. (Eastern time), Monday, September 16.
Visit this page to type in a comment or upload a Word document or PDF.
In the 15 years since MEI launched Home Dialysis Central, the numbers of home dialyzors have increased:
PD - from 27,748 to 51,057 (+84%)
Home HD - from 1,500 to 8,987 (+499%)
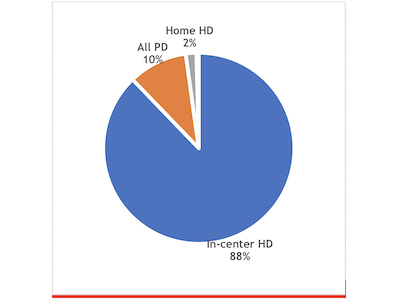
Because the dialysis population grew by 55% during the same period, the percentage of patients using home options has gained far less ground, however:
In-center HD dropped from 90.6 in 2004 % to 87.8% in 2016.
PD picked up much of the home dialysis increase, rising from 8.3% to 10%, despite the supply shortages a couple of years ago. The mix of PD has changed quite a bit: in 2004, about 63% of those on PD used a cycler, while in 2016, 82% did.
Home HD has grown over the 15-year period, from .5% in 2004 to 1.8% in 2016.
It is clear that in-center HD—the most costly and life-disrupting dialysis option, with the poorest survival—still retains its decades-long stranglehold over U.S. dialysis.
Three Ways the AAKHI Could Help
Improvement opportunities via the AAKHI that have occurred to me (note: I am a patient advocate and educator; not a clinician or a policy expert!) include:
1). Create a nephrologist certification in PD and one in home HD. Of the 140 or so U.S. nephrology fellowship programs, I’m told that only about a dozen require a hands-on rotation in PD or home HD. In fact, most don’t even require fellows to see standard in-center HD patients—just ICU patients. In our own national survey, 38% of 629 U.S. nephrologists reported feeling “not very well prepared” to care for dialysis patients when they took the certification exam. They knew home dialysis was better—94% of respondents would choose PD or home HD for themselves—but were not comfortable prescribing either for patients. Passing a certification exam could increase confidence in themselves as well as in their patients. Perhaps the International Society of Peritoneal Dialysis (ISPD) and the International Society of Hemodialysis (ISHD) could collaborate to develop a certification program.
2). Expand use of transitional care units (TCUs) to all new in-center HD patients.1 The TCU model of weeks of paced education and orientation dates back to the 1980s in Seattle, the birthplace of chronic hemodialysis.2 Rather than tossing terrified new patients (whether crash start, incident, or coping with failure of PD or a transplant) into an unfamiliar setting, the planned TCU approach offers hope, reassurance, and vital socialization into a self-management role. Patients who are not capable of benefitting from a TCU approach may still have family members who can—and what they would learn could help to guide appropriate decisions about initiating chronic dialysis. For either group, a TCU offers the potential to improve onboarding of new patients and ensure a consistent educational approach.
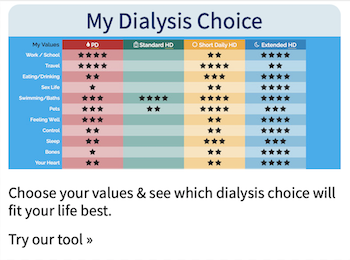
3). Map dialysis options onto patients’ lifestyle and values. When I first started to write this post, I was going to use the phrase “values-first” in the title. But, it turns out that value-first healthcare pays providers based on outcomes—so, it is really focused wrongly (in my opinion) on the values of care providers—not consumers! With any chronic disease, the choice of treatment needs to maximize quality of life and allow people to keep what matters most (which requires asking people what they value). In my experience, it’s shocking how rarely this happens. Clinicians may think they know what is most important to their patients—and tend to assume it’s survival. This is not always the case, and dialyzors are not a homogenous group. Each person has his or her own list of what brings them joy or makes them want to get up in the morning. Dialysis is too often thought of as a way to clean water and wastes out of the blood, and not as a highly intrusive medical intervention that affects every aspect of lifestyle. So, when the time comes for people to choose a dialysis option, we need to stop using a modality-first approach. Get to know your patients. Learn what is important to them:
Use My Life, My Dialysis Choice first, then offer details about the options. Taking this step will help to avoid errors like pushing PD on someone whose favorite activity is swimming or who wants to have a baby, or insisting that short daily home HD is a good choice for someone who works full-time.
Use the MATCH-D to determine what challenges could preclude particular option choices and develop tactics to overcome as many as possible.
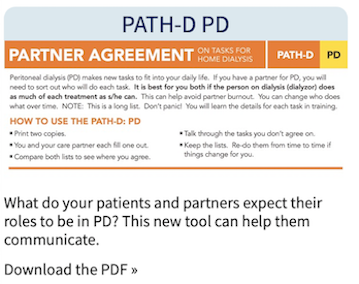
Have prospective home dialyzors and care partners each use the PATH-D-PD or PATH-D-HHD tool to see how they can divide the tasks of home treatment to avoid burden.
No doubt there are plenty of other excellent payment model suggestions that could help ensure that those who need dialysis have the information they need to choose a type that will let them live as well and as fully as possible. I hope you will share these in the comment section below, so they can be echoed by anyone who plans to comment publicly by September 16th.


Comments
John Agar
Jul 26, 2019 3:20 AM
Dear Dori
As you know, I made some (possibly inept) comments at last weeks’ KidneyViews blog by Elizabeth Witten ... see:
https://homedialysis.org/news-and-research/blog/319-what-the-em-advancing-american-kidney-health-initiative-em-aakhi-executive-order-may-mean-for-you
I will copy a (slightly) edited version of the same comment here:
The stand-out thing that bothers me about Trump’s Executive Order is the potential for huge unintended consequences. Home dialysis can only succeed if two ‘unmentioned’ and, I fear, ‘poorly recognised’ factors that seem to be missing from this rush-of-blood Executive Order dubbed the Advancing American Kidney Health Initiative (AAKHI).
1. A careful specialty-wide education process … not only of the patient going home, or (peculiar to the US) of a care-giver … though this education is crucial ... but of the professional staff [nurses and doctors] who must administer, oversee, advise, support, and empathise with their home patients.
2. An in-depth core understanding of the principles of dialysis - both of PD and HD - and how home dialysis allows any one individual’s dialysis program to be elevated from the subsistence care offered by in-facility dialysis programs [NB: the euphemism ‘adequate’ is sometimes used as a substitute for subsistence], to achieve optimum, best-in-class home dialysis outcomes.
I may be behind the times with my data now - though, somehow, I don’t quite think I am - but it was only 5 years ago that data was presented by Bob Lockridge (an unchallengeable US home HD expert from Lynchburg, WV) and by Dori Schatell (from Home Dialysis Central and the Medical Education Institute in Madison WI) that noted:
1. Less than 10% or US Fellow training programs actually trained for or exposed training Fellows to home dialysis [Bob Lockridge]
2. Only 3/100 questions on the Nephrology Boards Examination were about dialysis, dialysis principles, or dialysis management - let alone home dialysis … on which there were none! [Dori Schatell]
I fear that this lack in training, in exposure, in education, and in experience has not materially changed since that data was presented.
Throwing Executive Orders like the AAKHI at, and pouring Federal money on, home dialysis without prefacing and packing this with an intensive up-skilling effort into the basic groundwork, training, and lived experience of the professional practitioners who must advise, oversee, and manage dialysis at home will perilously risk a bottom-line driven rush to push patients home, without a matching expertise to manage them there.
This will inevitably generate worse, not better home outcomes for a great many unsuspecting patients.
Dialysis should not be about money - it should only be about outcome ... patient outcome. Home dialysis should be about patient empowerment, patient self-autonomy, and patient outcomes and not about saving money - though I fear the latter may be the hidden subtext of Trump’s AAKHI EO. US dialysis has always put profit first, and a leopard does not change its spots! It is hard to see any home incentivisation program being different.
Unless urgent and synchronous attention is given to nephrology training programs - for both physicians and nurses - I fear the laudable patient-directed goals of empowerment, self-autonomy, and outcome may be submerged in an ocean of poorly trained and executed programs. This would be to the long-term detriment of home care.
Further, good training requires an experiential base to build from ... and that base is sadly lacking. CMS fact-finding visits to Australia, New Zealand, Canada, the UK, Finland and Turkey would be wise - though US healthcare rarely lifts its gaze beyond its own shoreline.
If only the AAKHI had critically addressed the whole US reimbursement system by considering the game-changer proposal from Mel Hodge: see https://www.homedialysis.org/news-and-research/blog/153-kidney-caucus-letter-repayment-basis. But, sadly, it did not.
I fear that the dialysis companies will turn this new EO to their financial benefit - for as sure as eggs they will - and the patient ... again ... will be lost in the scramble for profit and 'the bottom line'.
Dori ...
Firstly, I suggest that your blog + any edited but identified comment (like this one) that are made in response, should be submitted by MEI by the due date as a collective response.
Secondly, I do not think any submission would be complete without reference to SONG-HD, and SONG-PD ... as both demonstrate the very different sets of ‘the things that matter’ between professionals and patients. While you refer in your blog to the marked differences in aspiration and emphasis between patients and doctors - with nurses somewhere in between - the SONG initiative gives a powerful study voice to your inference. It would be far more powerful if SONG-HD and SONG-PD could be represented.
John Agar
Clayton
Feb 12, 2021 10:25 AM